Phases of Physical Therapy
An Overview of Physical Therapy After Surgery
Diminishing swelling and pain, regaining range of motion, regaining strength, regaining endurance, and performing sports-specific exercises are the steps to full recovery. We define full recovery as the ability to do whatever you want with your shoulder without reserve, pain, or fear. Postoperatively, some people reach levels of function that are lower than others, depending on their goals and lifestyles. A person's overall function after shoulder surgery depends on many factors: the amount of trauma found and treated during the surgery, the body's reaction to the surgery, the body's inherent (genetic) potential to heal, the quality of the tissue within the joint, the quality of the repair during the surgery, the person's tolerance of pain, the motivation of the physical therapist and patient, and the home exercises performed by the patient. At times, patients will stop getting better before gaining a level of function that permits participation in sporting events or before reaching their pre-injury joint function.
Physical therapists utilize their knowledge of the human body, their hands, and modalities (electronic, ultra-sonographic, continuous passive motion, etc.) to facilitate blood flow to the area, to encourage fluid reabsorption in the area to diminish swelling, and to help with pain relief. They help educate the patient about exercises and activities that can be done to increase function and to decrease pain.
As a general rule of thumb, prior to a home exercise program and physical therapy sessions, warming the shoulder makes tissues more pliable and flexible. This is an activity to help alleviate stiffness. The warmth increases blood flow to the area and will help soften up some scar tissue formations as well as allow the patient to perform the exercise programs.
There may be bleeding or increased fluid in the area after the movements of therapy or home exercises. In addition, at therapy or during home exercises the joint may reach places it has not been in quite some time. After the exercise program is finished, one can utilize ice to help cool down the stretched-out tissues and diminish the pain and the swelling that may ensue if small scar tissue bands have been broken during the exercise.
THE FOUR PHASES OF PHYSICAL THERAPY ARE:
1. Acute Phase
2. Intermediate Phase
3. Advanced Strengthening
4. Return to Sports

Phase 1:
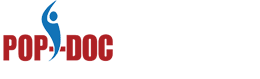
Reduce pain and swelling Rehabilitation begins one to two weeks postoperatively. Passive range of motion, manual therapy, initiation of gentle rhythmic stabilization exercises, scapular stabilization exercises and modalities are utilized as needed to reduce pain and increase range of motion. Instruction in the use of a sling and modification of activities of daily living are reinforced to maintain and/or protect the integrity of the repair.
Phase 2:
Initiate active range of action and activity tolerance Exercises are introduced to increase active motion while allowing for continued healing of soft tissue. Full passive range of motion is gradually restored during this phase. Manual therapy and modalities are used as needed to continue to reduce pain and inflammation. The use of a sling is gradually diminished, with instruction to not overstress the healing tissues.

Phase 3:
Increase muscle strength and endurance The patient should have full passive and active range of motion. Joint exercises for strength and endurance are progressed here and more dynamic joint stabilization exercises are introduced. Exercises include eccentric contractions, proprioception and neuromuscular re-education, and multi-joint and multi-planar endurance exercises. Exercise selection is based on patient goals and activity/occupational demands. Manual therapy and modalities are used as needed.
Phase 4:
Return to sport Advanced strengthening to increase muscle strength, power and endurance are performed so the patient can attempt to return to his or her previous level of sport participation. Maintenance of full, non-painful active range of motion and full strength are important. Plyometric activities and sports-specific loads are applied to the joint. Plyometric exercises enhance dynamic stability and proprioception and should be chosen individually based on sport-specific demands.